You can’t price a new network with an old operating model
Why aggressive premium reduction requires redesigning how care actually flows

Why aggressive premium reduction requires redesigning how care actually flows
Executive summary
If there is a common thread across today’s health system and health plan strategy discussions, it is the challenge of organizing primary care and specialty physicians into a high-performing network that can simultaneously achieve three objectives:
- Enable significant premium differentials up to 20 percent below comparable market offerings, driven by sustained medical cost improvement rather than benefit erosion
- Deliver concierge-level access and patient experience at that lower price point
- Accelerate throughput gains, shifting appropriate care away from constrained inpatient acute capacity toward ambulatory, virtual, and outpatient settings
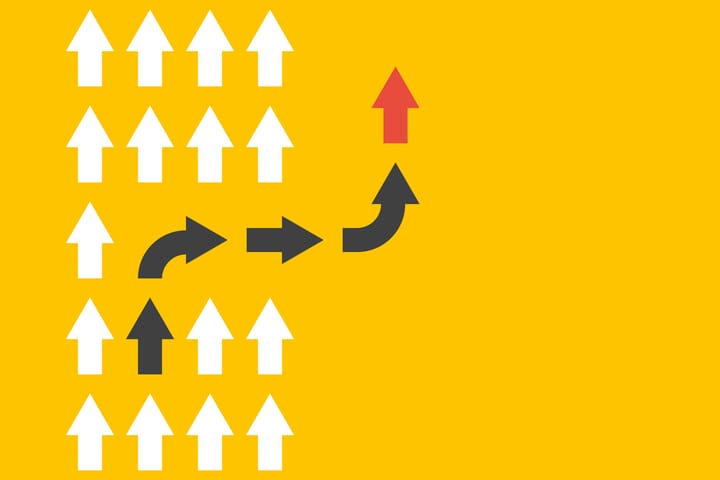
The difficulty of achieving any of these outcomes is great. Delivering all three is not possible without a fundamental change in how we deliver and finance care in ways that require health insurers and care delivery enterprises to work together differently.
Problem statement
Two questions frame the challenge for leaders:
- How can insurers and providers work together to design an operating platform that predictively directs members to the right care, at the right time and place, the first time?
- How do we accelerate the removal of friction and low-value steps embedded in care journeys, while deploying limited clinical capacity more deliberately across the network?
Answering these questions requires big thinking unconstrained by current-state realities. My observation is that a material premium reduction (on the order of 20 percent), combined with radically improved member access and more efficient use of scarce provider capacity, cannot be achieved through incremental levers alone.